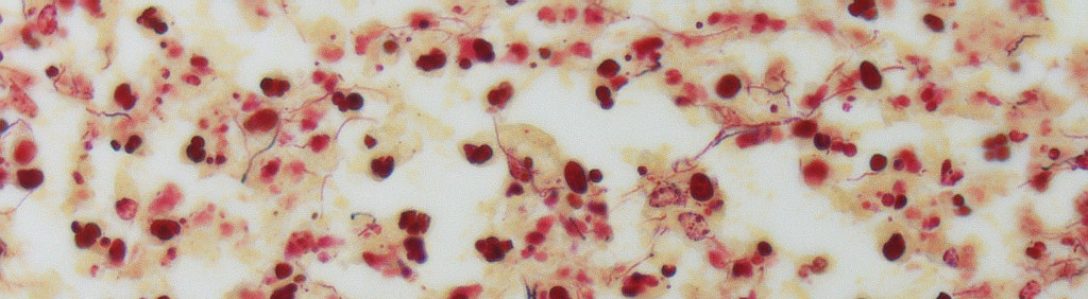
In the world of combating disease, it is important to consider two things: we can either destroy the threat or we can alter our soldiers to be stronger. Altering soldiers is exactly what CAR T-cell therapy does. In this method of cancer treatment, a patient’s T cells are removed from their body. Next, they are genetically altered to have more receptors on their surface. These receptors are known as chimeric antigen receptor cells, or CAR T cells. Following a brief bout of chemotherapy, these altered T cells are introduced back into the patient’s body and target CD19, a protein commonly found on the surface of cancer cells. This allows the CAR T cell to bind to the cancer cell and kill it with ease.
Although this seems like a full proof method of fighting cancer, there are many adverse side effects, such as fatigue, nausea, headache. These symptoms can escalate into more nasty conditions, such as cardiac arrest and renal insufficiency. Additionally, patients may develop tumor lysis syndrome, which is a metabolic complications that can occur and cause organ damage. Most of these side effects can be managed with drugs. When compared to the usual health risks of chemotherapy and other standard cancer treatments, these side effects are about the same level of severity.
This type of T cell therapy has a high success rate, with over 80% of patients experiencing a complete or partial response. Additionally, many young children tested with CAR T-cell therapy had their cancer go into remission. Early results of CAR T-cell therapy for treating lymphoma and other blood cancers are promising, with patients whose cancer was previously untreatable going into remission. However, these successes must be applied to larger numbers of patients to discover more side effects and how efficient the treatment really is. This therapy is promising, but is more expensive than standard cancer treatments and needs more testing.